Natural Choices are indeed better.. especially when proven by science
Milk Calcium, Phosphorus and Vitamin D Tablets







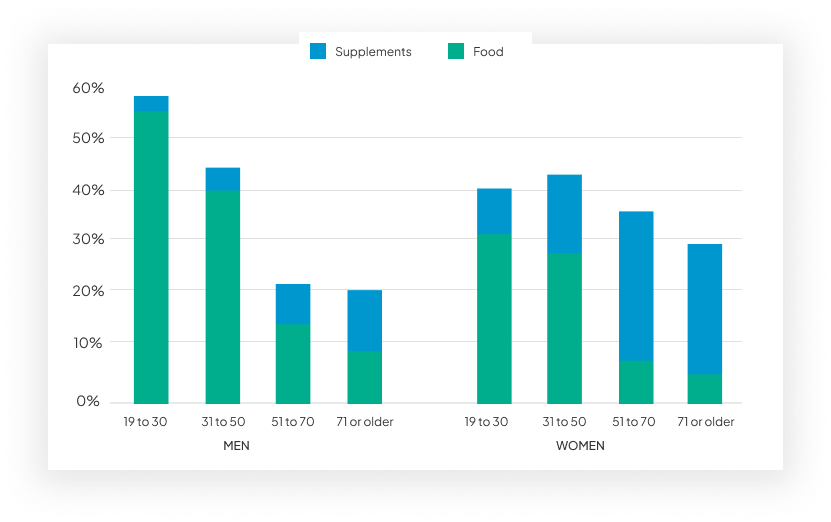
Although calcium intake is indeed a risk factor; Over the age of 50 in Women, majority of calcium intake is through supplementation.


| Milk Calcium | Calcium supplement | |
|---|---|---|
| Drug Interactions | The calcium is protected by the Casein phosphopeptides (CPP) and hence interactions are far fewer. | Calcium supplements can interact with several medications: the absorption of calcium from calcium carbonate is reduced by proton pump inhibitors, while calcium supplements may interact with antibiotics, thiazide diuretics, digoxin and phenytoin. |
| Absorption | Active and Passive transport. Casein phosphopeptides (CPP) bind calcium and therefore protect it against precipitation with anions such as phosphates in the small intestine. The net result is an increase of passive calcium absorption in the ileum | Transcellular pathway (active transport) account for majority of absorbtion. |
| Vitamin D deficiency | Can be also absorbed by the influence of lactose in the distal small intestine via the paracellular route. Thus milk can provide calcium with “ensured absorbability” which is generally insensitive to external factors. | Impacts calcium absorption. |
| Absorbtion inhibitors | No Effect of inhibitors, as calcium is protected in CPP. | Supplemental calcium absorbtion is inhibited by phytates, oxalates, uronic acids or polyphenols in diet. |
| Calcium utilization | The availability of calcium for bone mineralization appears to be greater for dairy foods and the effects are longer lasting. | Absorbtion of calcium is non inferior to dairy calcium but utilization in bone is less. |
| Phosphorous content | Increased inorganic phosphate intake leads to decreased urinary calcium and increased calcium retention. calcium and inorganic phosphate in a ratio close to that found in dairy products leads to positive effects on bone health. | Conventional supplements have no phosphorous. |
| PPI usage/ achlorhydria | Milk calcium is bound to peptides and proteins making it efficacious. | Impaired acid levels impact calcium absorbtion. |
| Meal Effect | Provide an almost complete diet whose consumption provides a “meal effect”. This fosters the absorption of calcium and provides a simultaneous intake of phosphorus that is essential for bone deposition. | Calcium supplements do not contain the additional nutrients—including protein, phosphorous and magnesium. |
In 111,184 pregnant women study, the consumption of higher amount of Milk & related products was associated with a reduced risk of small-for-gestational age(SGA) (OR = 0.69,95%CI: 0.56-84) and low birth weight infants (OR= 0.63, 95 % CI: 0.48% - 0.84 )
Calcium reduces the risk of preterm delivery in women with low calcium intakes by 24%. The mode of action of calcium is that it reduces parathyroid release and intercellular calcium so reduces smooth muscle contractility.
The skeleton of a new baby contains approximately 20-30 g of calcium. The increase in calcium absorption is directly related to maternal calcium intake . During pregnancy 57% is absorbed during the second trimester and 72% during third trimester.
Daily supplementation of elemental calcium in pregnancy was associated with 66.7% risk reduction in developing preeclampsia. Low calcium intakes during pregnancy may stimulate PTH secretion, increasing intracellular calcium and smooth muscle contractibility and/or release renin from the kidney, leading to vasoconstriction and retention of sodium and fluid.
Fetal calcium levels suggest that ionized calcium is transferred from the mother to the fetus at a rate of 50mg/day at 20 weeks of gestation to a maximum of 330 mg/day at 35 weeks of gestation.
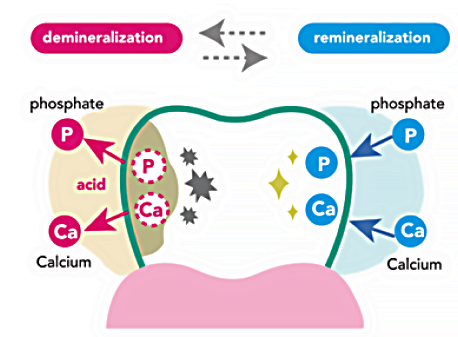
When combined with calcium and prosperous, casein creates a protective protein film over the enamel surface of the tooth. This has the ability to reduce the risk of tooth decay and decrease enamel strength.
A 10-fold increase in diary calcium intake was significantly associated with a decreased risk of tooth loss (incidence-rate ratio 0.32, 95% confidence interval 0.15 - 0.68)
Diary products are good source of calcium, the casein phosphopeptides enhance calcium absorption and mineral retention.
Higher daily intakes of milk may be protective against periodontitis and was inversely associated with severity of periodontal attachment loss.
For the non-pharmacological management of osteoporosis, single-nutrient supplements will frequently be inadequate and preference should go to the use of complete supplements or complete foods such as dairy products.
Calcium supplementation should only be targeted to those who do not get sufficient calcium from their diet and who are at high risk for osteoporosis and/or fracture.
Dairy calcium is non-inferior to calcium from mineral salts, the availability for bone mineralisation appears to be greater for dairy foods and the effects are longer lasting.
Postmenopausal women, those randomised to dairy calcium had greater improvements in arm, pelvis, total spine and total-body bone mineral density (BMD) than those receiving calcium supplements in one trial.
Greater increases in insulin-like growth factor-I (IGF-I), which favours bone formation, have also been reported for dairy compared with calcium supplements.

Milk Calcium (Casein phosphopeptide complex) ............. 1200 mg
equivalent to bio optimized
Calcium ......... 300 mg
Elemental Phosphorous .......................... 150 mg
Cholecalciferol
(Vitamin D3) BP .................. 400 IU
